To facilitate understanding of breastfeeding and problem-solving, we have compiled accurate information from various sources. The following answers are referenced from the Department of Health or reviewed by International Lactation Consultants (IBCLC) Dr. Tsang Wai Man, Dr. Fung Wai Han, and Ms. Wong Nga Wai.
If you have other breastfeeding inquiry, feel free to contact us or seek assistance from healthcare professionals.
Pregnancy
Breast massage during pregnancy does not help with postpartum milk production and may cause breast discomfort due to overstimulation. Starting breastfeeding early and correctly after birth is the most effective way to increase milk supply.
Breast massage during pregnancy does not help with postpartum milk production and may cause breast discomfort due to overstimulation. Starting breastfeeding early and correctly after birth is the most effective way to increase milk supply.
Breast size is influenced by the amount of fat, and smaller breasts do not necessarily mean less milk production.
No, nothing is more effective than starting frequent breastfeeding soon after birth to build up milk supply.
Babies should latch onto the areola, not the nipple, so nipple shape does not have an absolute impact on breastfeeding.
After birth, babies should be encouraged to learn to suckle as soon as possible:
- Allow skin-to-skin contact with the newborn to help them naturally find the breast and latch on.
- Avoid using bottles or pacifiers (including soothers) to prevent nipple confusion. Expressed milk can be fed to the baby using a cup or spoon.
- If there are difficulties with breastfeeding, seek appropriate professional help early (such as from a lactation consultant at a health center or hospital).
Some mothers worry that continued breastfeeding during pregnancy may stimulate uterine contractions and lead to premature birth. However, research shows that breastfeeding during pregnancy is not related to miscarriage, preterm birth (less than 37 weeks), or low birth weight.
If there is a history of preterm birth, pregnancy complications like preeclampsia, abnormal bleeding, or twins, consult a doctor.
Mothers who have had a cesarean section can start breastfeeding immediately if they are fully awake and the baby is in good condition.
Mothers can adopt any comfortable position, such as side-lying or football hold, to help alleviate wound pain.
If the mother is a hepatitis B carrier, healthcare professionals in Hong Kong will administer hepatitis B immunoglobulin and hepatitis B vaccine to the baby after birth to prevent infection. Therefore, mothers can breastfeed without worrying about transmitting the virus through breast milk.
During pregnancy, a mother’s antibodies are transferred to the fetus through the placenta. After birth, these antibodies are depleted by about six months.
In the first two to three years after birth, babies have a low ability to produce their own antibodies and are susceptible to infections. Breast milk contains natural antibodies, live immune cells, enzymes, etc., which help reduce the risk of infectious diseases.
Rooming-in refers to the hospital arrangement where the mother and baby stay in the same room after delivery, allowing the mother to breastfeed and comfort the baby at any time. This helps establish milk supply and provides a sense of security for the baby.
- Rooming-in allows mothers to see early hunger cues from the baby and respond quickly to their needs. This helps the baby practice latching with more patience, increases the efficiency of learning to breastfeed, and reduces the chance of nipple damage for the mother.
- With the baby nearby, mothers can learn to observe various signals from the baby and respond immediately, reducing crying. The baby can quickly become familiar with the mother’s voice and scent, strengthening the mother-infant bond.
- Being with the baby can reduce separation anxiety for the mother and provide peace of mind.
Newborn
In the early stages of breastfeeding, mothers may feel slight discomfort or mild pain in the nipples. If the baby latches correctly, the pain should quickly subside. Persistent pain or nipple damage usually indicates incorrect latching. A correct latch should not cause significant pain.
If there is pain or damage, seek help early.
Of course. Applying breast milk to the wound and keeping it dry should help it heal quickly.
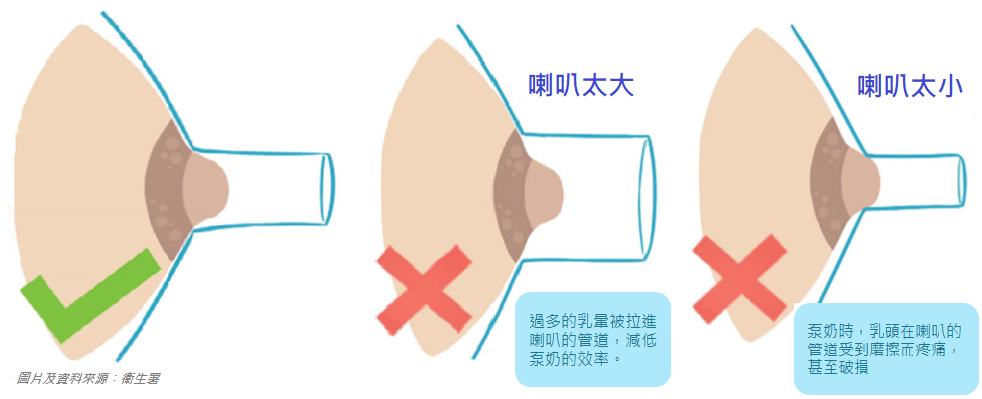
Nipple damage is usually caused by incorrect latching or an unsuitable breast pump flange size.
If there are difficulties with breastfeeding, seek appropriate professional help early (such as from a lactation consultant at a health center or hospital).
More information:
- How to choose a breast pump?(Department of Health)
Colostrum is thicker and helps the baby learn to suck, swallow, and breathe. The small quantity of colostrum matches the marble-sized stomach capacity of a newborn.
Learn more:
A fully breastfed baby who is getting enough will…
- Gradually gain weight; exclusively breastfed babies should gain at least 0.5 kg per month in the first three months.
- Appear satisfied after breastfeeding
- Show swallowing movements while sucking (observe the area below the ears and jaw)
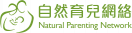
- Have enough wet and dirty diapers
A newborn’s stomach is only marble-sized (about 5 to 7 ml capacity), which matches the amount of colostrum, so not much milk is needed.
Mothers should not wait for milk supply to come in before breastfeeding. Early breastfeeding can help the body build up milk supply quickly. If the baby has enough wet and dirty diapers, formula supplementation is unnecessary.
Learn more:
Every mother’s experience and situation are different. Some mothers do not feel significant breast fullness, but as long as the baby is getting enough milk, it’s fine.
Learn more:
Every mother and baby is unique. Babies may want to breastfeed not only because they are hungry but also because they are thirsty, want to be close to their mother, or want to sleep. Therefore, the duration and frequency of breastfeeding sessions may vary. Observe the baby’s condition to decide when to start and stop breastfeeding, without time restrictions.
Learn more:
- How to know if the baby is getting enough when breastfeeding?
- Hunger cues in babies (Department of Health)
In the early stages, using both breasts for each feeding provides enough stimulation to establish milk supply.
Once milk supply is established, mothers can feed from one breast until it is soft. If the baby is still not satisfied, they can switch to the other breast. If the baby is satisfied after feeding from one breast, feeding can stop.
Yes, frequent breastfeeding allows the baby to consume more breast milk and helps excrete bilirubin quickly, speeding up the resolution of jaundice.
Some breastfed babies may have prolonged jaundice, known as “breast milk jaundice”. “Breast milk jaundice” does not affect the baby’s physical or brain development and will naturally resolve within two to three months.
If the baby is introduced to bottle feeding too early, they may refuse to latch onto the breast. Mothers can try the following methods to help the baby return to breastfeeding:
- When the baby is just waking up and not too hungry, the mother can hold the baby with skin-to-skin contact to stabilize the baby’s emotions and stimulate the rooting reflex.
- Let the baby lie on the mother’s breast and find the nipple on their own. Once the baby latches onto the breast, hold the baby close.
- If the baby becomes impatient, do not force it and try again later.
Observe the baby’s early hunger cues (e.g., opening their mouth to search for food, putting their hand to their mouth). Feeding at these times usually results in better feeding. If you wait until the baby is very hungry (e.g., crying), they may not suckle as well.
Learn more:
- Hunger cues in babies (Department of Health)
A correct latch involves the baby taking in the entire nipple and most of the areola, and you will see:
- A wide-open mouth with no overlap at the corners
- The lower lip turned outward
- The chin touching the breast
- More of the areola visible above the baby’s mouth than below
- Cheeks rounded and full during sucking
- Rhythmic sucking with occasional pauses
- After feeding, the baby will release the breast and appear satisfied
- After feeding, you will feel that the breast is softer than before feeding
Nipple after sucking:
- Correct latch: The nipple remains unchanged or is cylindrical
- Poor latch: The nipple is flattened, seek professional guidance
Watch video:
- Breastfeeding Attachment (Global Health Media)
13. Are the Benefits of Breastfeeding Directly and Bottle-Feeding Breast Milk the Same for the Baby?
Breastfeeding is not just about providing food and nutrition. The contact between mother and baby during breastfeeding strengthens their bond and closeness, releasing oxytocin, the “love hormone”, which has various benefits for both mother and baby.
Oxytocin can help:
Baby:
- Stimulate emotional intelligence, promote brain development, and help grow into a happy and confident child
Mother:
- Relax the body and mind, maintain a happy mood, enhance maternal love, and positively impact parenting skills
- Direct breastfeeding helps implement responsive feeding
- Allows the baby to control their intake, reducing the risk of overeating and lowering the chances of obesity and diabetes in the future
- Sucking on the breast trains the baby’s oral muscles, reducing the chance of dental misalignment (e.g., buck teeth)
Continuous
During teething, babies may bite the mother while breastfeeding due to itchy gums. The mother can immediately remove the nipple and, in a slightly more serious tone than usual, tell the baby that this is not right. Additionally, the mother can remove the nipple when the baby is about to fall asleep to avoid accidental biting.
If the baby’s gums are red and swollen, provide a chilled and clean “teething ring” or a damp, clean cloth for the baby to bite on to relieve gum discomfort before breastfeeding, reducing the chance of being bitten.
After the first month, the frequency of bowel movements may decrease, and the baby may go several days without a bowel movement. If the baby is not vomiting or bloated, passes gas daily, and has soft stools, it is normal.
A growth spurt is when the baby suddenly demands more frequent feedings, and wet diapers increase accordingly. This can last from a few days to over a week. The mother can feed according to the baby’s needs, and milk supply will increase to meet those needs.
Generally, when a baby suddenly increases feeding frequency, it is due to increased demand for milk, not a decrease in the mother’s milk supply. This is commonly seen during a “growth spurt”.
Learn more:
Starting from 3-4 weeks after birth, the baby’s milk intake will gradually stabilize. Some babies may reduce their intake or feeding frequency. Mothers or caregivers can feed according to the baby’s needs.
After the first 3-5 weeks of milk regulation, the mother’s milk supply stabilizes. Compared to before, even if the milk supply meets the baby’s needs, the feeling of fullness in the breasts becomes less noticeable.
Common illnesses like colds and gastrointestinal issues are not transmitted through breast milk. In fact, the antibodies in breast milk can enhance the baby’s immunity when the mother is sick. Mothers can continue breastfeeding. Pay attention to hygiene, wear a mask if necessary, and thoroughly clean hands before holding the baby to prevent transmission.
Mothers should not worry about medications affecting breast milk quality and should seek medical advice promptly.
Learn more:
Most medications do not affect breastfeeding, and there are medications available for common illnesses that are compatible with breastfeeding. Mothers should inform doctors or Chinese medicine practitioners that they are breastfeeding to ensure the prescribed medication does not affect the baby.
If there are concerns about Western medicine, mothers can call the Department of Health’s breastfeeding hotline at 3618 7450 for inquiries.
Breast milk contains a large number of beneficial gut bacteria and antibodies. When a baby has diarrhea, breastfeeding should continue to speed up recovery. Ensure the baby is adequately hydrated to prevent dehydration.
If the condition is severe or worsens, see a doctor promptly.
Some exclusively breastfed babies may have pasty, looser, or more frequent stools. The color may be yellow, brown. As long as the stool is not watery or foamy, it is fine.
If there are concerns, consult a health center or healthcare professional.
When some milk is not effectively expelled from the breast, leading to one or more milk ducts being blocked, it results in a blocked milk duct. The mother may feel lumps or hardness in the breast but may not necessarily feel pain.
If a blocked milk duct is addressed early, it can prevent the development of mastitis. If the blockage persists for more than 24 hours or symptoms worsen, such as fever, fatigue, severe pain, or redness, it may be mastitis. Seek advice from healthcare professionals or a maternal and child health center. Continue breastfeeding to maintain milk flow and prevent worsening of the blockage.
Learn more:
If a blocked milk duct does not improve or symptoms worsen, such as fever, fatigue, severe pain, or redness, it may be mastitis. Seek advice from healthcare professionals or a maternal and child health center.
During mastitis, mothers can continue breastfeeding. Inform the doctor that you are breastfeeding, as many medications are safe for breastfeeding. The best way to improve blocked ducts/mastitis is to ensure milk is expelled from the breast. The following methods can help maintain milk flow and prevent/improve blockages:
- Continue to let the baby latch onto the breast
- Ensure the baby latches correctly (video: Observe mouth shape)
- Try different breastfeeding positions (video: Breastfeeding positions)
- Increase the frequency of breastfeeding
- Mothers who exclusively pump should increase pumping frequency
Before breastfeeding or pumping, use the following methods to stimulate the let-down reflex and help milk flow:
- Skin-to-skin contact: Place the baby on the mother’s chest without clothing barriers
- Gently massage the breast, avoiding excessive force to prevent increased swelling
- Warm compress on the breast (less than three minutes); prolonged or excessive heat can increase swelling
- Avoid wearing tight or underwired bras, as they can obstruct milk flow
Relieve pain caused by engorgement:
- If there is still pain after breastfeeding, apply a cold compress to the breast to help reduce swelling.
- You can also freeze cabbage leaves, crush them, and apply them to the breast until the leaves are no longer cold, then discard. This can also relieve engorgement for mothers with excessive milk production.
White spots on the nipple may be caused by a blocked milk duct opening at the nipple.
If the mother does not feel pain, no treatment or handling is necessary. If there is pain, try applying cooking oil with a cotton ball to the nipple before breastfeeding or pumping to soften the skin, then clean it before letting the baby latch. If the situation does not improve, consult a maternal and child health center.
If the white spots are larger or there are multiple spots and persistent pain, consult a maternal and child health center.
- Clean hands before breastfeeding, pumping, or touching the baby
- Take appropriate precautions before direct breastfeeding or touching the baby, such as wearing a surgical mask
- Keep all surfaces you touch clean
- If unable to breastfeed or temporarily stop breastfeeding, pump regularly to avoid blocked ducts and mastitis
- Clean hands before touching pump or bottle parts, and wash all parts after each use
Work, Storing Milk, Expressing Milk
There are various designs and operating modes of breast pumps available on the market. Mothers can consider the following aspects:
Operating characteristics
- Frequent and regular use: Choose an electric pump
- Short pumping time: Choose a double pump
- No power source or fixed pumping location: Choose a battery-operated pump
Properly sized flange
- The flange should fit snugly against the breast
- No friction when the nipple is drawn into the flange
- Little or no areola is drawn into the flange
- No pain
- Breasts gradually become softer
More reference materials:
- Comprehensive understanding of “breast pumps” (Department of Health)
Some mothers worry that the amount of milk pumped during work may not meet the baby’s needs, so they establish a breast milk reserve (storing milk in the freezer for future use).
Mothers who need to establish a breast milk bank can express a small amount of milk before or after breastfeeding, then mix several expressed milk portions at the same temperature as needed for storage. For example, express 20ml of milk each time, store it in the refrigerator, and mix three expressed and already frozen milk portions (20ml x 3) into one container for freezer storage.
Note: Do not over-pump milk to avoid excessive milk production, which can lead to blocked ducts.
If mothers can arrange time to pump milk after returning to work, storing a few meals’ worth of milk for emergencies is sufficient. Excessive storage is unnecessary to avoid waste.
Some babies may refuse frozen milk due to a different taste, wasting the mother’s effort if too much is stored.
Every company’s environment is different. If there is no vacant room for pumping, mothers can consider using a nursing cover or shawl to pump at their desk. Some mothers may go to a nearby nursing room to pump.
Thawing Frozen Milk
Move frozen milk from the freezer to the refrigerator (normal compartment) the night before use to thaw slowly. To speed up thawing, place the frozen milk in a container of water and then in the refrigerator, or rinse the milk bottle with water.
Warming Breast Milk
Refrigerated milk can be consumed directly. If needed, place the milk in water below 55°C to warm it.
Learn more:
Tips
- Frozen milk should be consumed within 24 hours after leaving the freezer
- Thawed milk should not be refrozen
- Thawed and warmed milk should be consumed within one hour
- Do not use a microwave to warm breast milk, as uneven heating can burn the baby
- Excessive heating of breast milk can destroy nutrients
Frozen breast milk may separate into layers, with the top layer being fat and appearing pale yellow. This is normal. Shake the milk before feeding.
Mothers do not need to worry about the amount of fat layer, as breast milk composition adjusts to the baby’s growth needs, weather, environment, etc.
Learn more:
Generally, mothers can only pump a portion of the milk produced by the breast, so using pumping to assess milk production or the baby’s intake is inaccurate.
Some mothers use pumping to assess the baby’s intake, but generally, mothers can only pump a portion of the milk produced by the breast, so this method is inaccurate.
Every baby’s intake is different. Mothers can first let the baby try a bottle to test the approximate amount needed.
When preparing stored milk, divide the breast milk into different portions (e.g., some 30-50ml portions, some 90-100ml) to allow caregivers to mix different amounts according to the baby’s needs.
Some babies do not like bottle feeding and may refuse to eat while waiting for the mother to return for breastfeeding. Caregivers can try feeding the baby with a small cup or spoon. If the baby’s intake is still low but the baby increases feeding frequency when the mother returns home and gains weight normally, there is no need to worry.
Diet
Breastfeeding mothers only need an additional intake of about 500 calories per day.
Diet tips:
- Variety in food and a balanced diet
- No need to overeat
- Ensure adequate hydration, but no need to drink excessively
- If supplementation is needed, use medicinal herbs under the guidance of a registered Chinese medicine practitioner
Breastfeeding mothers should prioritize a balanced diet unless the baby is allergic to certain foods, such as when the baby has allergic reactions after the mother consumes a particular food multiple times. Otherwise, there is generally no need to avoid specific foods.
If a baby is suspected of having an allergic reaction, see a doctor promptly.
There are many claims about foods that reduce milk supply, but most lack scientific or traditional evidence.
Traditional texts support the use of Chinese medicine “”fried malt”” as a milk-reducing food, which is unrelated to regular foods like “”malt”” or “”malt””. Modern research shows significant effects only under high consumption.
If mothers are unsure whether a food affects milk supply, they can try eating a small amount first and decide based on their body’s reaction. Even if milk-reducing foods are accidentally consumed, there is no need to worry. Maintaining or increasing breastfeeding or pumping frequency will not significantly affect milk supply.
Breastfeeding mothers who need to take Chinese medicine or supplements should consult a registered Chinese medicine practitioner.
Every mother’s physical condition is different. Some mothers may not be suitable for supplementation. If you wish to use Chinese medicinal herbs to regulate your body, consult a registered Chinese medicine practitioner first and avoid self-medicating.
Common Myths
Regardless of the material, a very small amount of nutrients will stick to the bottle, but the remaining nutrients are still sufficient.
Due to hormonal influences, some mothers may experience a temporary drop in milk supply during the first few days of menstruation. This is temporary, and generally, mothers can restore milk supply by breastfeeding or pumping more frequently.
Simply press the nipple gently with a finger or cloth for a moment, and the leaking will stop.
Mothers who need to store milk for work can collect the leaked milk in a clean container and store it according to guidelines.
Yes, these do not affect breast milk quality.
Yes, these do not affect breast milk quality.
However, some babies may be sensitive to smells and refuse breastfeeding if the mother’s body odor changes after using scented products.
Babies grow and gain weight rapidly, and night feeding is necessary both physiologically and psychologically. Every baby’s needs, characteristics, and preferences are different, so mothers should feed according to their baby’s needs.